Information on the treatment of Snoring, Sleep Apnea, Excessive Daytime Sleepiness and other Sleep Disorders by Houston, Texas Neurologist and Sleep Medicine Specialist Jerald Simmons M.D. If you suffer from sleep problems, Dr. Simmons and his staff at CSMA can provide relief with three state of the art sleep medicine centers in the greater Houston area.

Monday, December 23, 2013
New Gallup Poll Data Suggests 40% of Americans Don't Get Enough Sleep
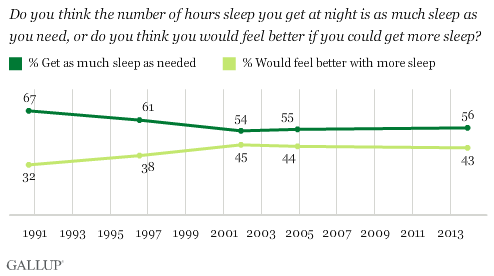
A new Gallup poll shows that 40% of Americans get less than seven hours of sleep per night- a figure largely unchanged from the 1990s and 2000s.
The poll is based on telephone interviews conducted Dec. 5-8, 2013, with a random sample of 1,031 adults, aged 18 and older, living in all 50 U.S. states and the District of Columbia.
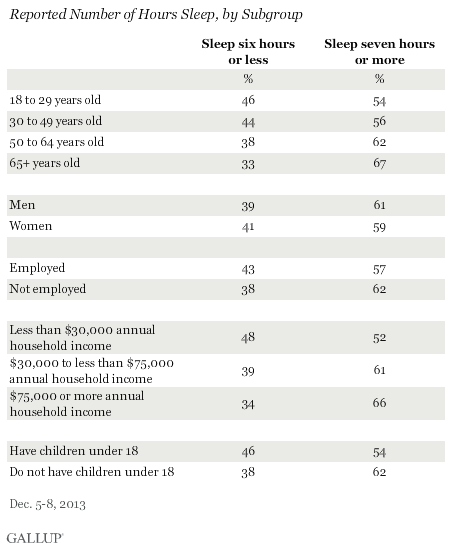
56% of Americans say they get as much sleep as needed, while 43% say they would feel better if they got more sleep. The percentage who say they get sufficient sleep has been in the mid-50% range since 2001, but was much higher in 1990. Americans aged 65 and older report getting the most sleep, with 67% getting seven or more hours per night. Each younger age group gets less sleep, down to 54% of 18- to 29-year-olds who report getting seven or more hours. Nearly half of 18- to 29-year-olds get less than the recommended amount of sleep.
Medical studies have related a lack of sleep to health problems and cognitive impairment: experts typically recommend seven to nine hours sleep for adults.
The indirect cost of sleep disorders is estimated at 41 billion dollars per year from lost productivity, 17 to 27 billion dollars per year from motor vehicle accidents, 7 billion dollars per year in work-related accidents and 2 to 4 billion dollars per year in home and public accidents (Stoller MK Clin Ther 1994:16 873-897). These figures do not even take into account the added morbidity caused by the physiologic impact from sleep disorders. Unfortunately, Sleep, a process which consumes about one third of our life and which has a spectrum of abnormalities which can hinder our daily living, has received so little attention in our medical education system.
For more information on the importance of proper sleep hygiene, The Societal Sleep Problem and sleep related illness please visit the HoustonSleep.Net.
References:
Gallup.com: In U.S., 40% Get Less Than Recommended Amount of Sleep
Methodology, full question results and trend data
Friday, December 13, 2013
Poor Sleep is Frequently at the Root of Fibromyalgia
For decades, doctors have been challenged in treating patients with a condition known as fibromyalgia. Patients with fibromyalgia complain of pain in various parts of their body, and evaluation by the doctor does not identify any physical cause. There are no inflammation or arthritic changes in the bones to explain the daily difficulties with pain. More than 12 million Americans have been labeled with this diagnosis and treatment options have been limited; for the most part it has consisted of pain medications or medications that dull the nerve pain transmission from around the body to the brain. These medications frequently cause side effects including drowsiness, and their benefits lessen over time.
A new direction in the management of fibromyalgia stems from our growing knowledge of this mysterious disorder. Dr. Jerald H. Simmons, neurologist and founding director of Comprehensive Sleep Medicine Associates (CSMA), says that fibromyalgia is a condition in which the brain's pain-filtering system is fatigued and does not function correctly: "Our brains constantly filter out signals coming in from the nerve fibers throughout the body. This allows us to function without feeling every little impulse coming from all of the nerves. When we sleep, this filter in our brain restores itself in preparation to function throughout the next day. When we are sleep-deprived or have not gotten proper sleep, the filter system begins to malfunction and signals from the nerves that should have been filtered out instead get into the brain and create the sensation of pain."
Another way to describe this is that our pain threshold is lowered by poor sleep, and this relationship between sleep and pain has become increasingly dear. As it turns out, many patients with sleep disorders who have also been identified as suffering from fibromyalgia experience resolution of their fibromyalgia pain as a result of treatment of their sleep disorder. The link between sleep and other conditions has become increasingly clear. "If we improve sleep in fibromyalgia patients, we have seen that the pain improves as well," Dr. Simmons says. "Common sleep disturbances such as obstructive sleep apnea, restless legs syndrome or upper airway resistance syndrome seem to be underlying causes of patients' fragmented sleep. Many of these patients also complain of chronic fatigue syndrome, further implicating sleep disruption as a contributing factor. I have had excellent results from identifying the root of the disrupted sleep and then treating the sleep disturbance."
Dr. Simmons uses a new approach to treat patients with fibromyalgia that have not been identified as having another sleep disorder; it involves Zyrem, a medication originally used for treating narcolepsy. "Now that I'm on Zyrem, I feel better than I have in 20 years," said Nancy Schweining, one of Dr. Simmons' patients. "My pain is gone and I feel like I have my life back." Dr. Simmons expects more doctors to recognize the proper use of this medication, which he said enhances Sleep Wave sleep in patients with fibromyalgia.
If you or someone you know suffers from fibromyalgia, consider the possibility that poor sleep may be at the root of the condition. Evaluation can be provided by Dr. Simmons and his staff at CSMA's sleep centers throughout Greater Houston by calling 281-407-6222 or by visiting www.HoustonSleep.Net.
Thursday, November 21, 2013
New Study Shows That Changes in Your Sleep Schedule May Help You Lose Weight
A study led by Bruce Bailey, professor of exercise science at Brigham Young, followed 300 female college students ages 19 to 26 who were given
activity trackers to monitor their movements and activities including
waking and sleeping times. The participants were assessed for body composition before and after the one-week study period. Although previous research has shown that not sleeping enough can have an effect on
weight, the new study found that
consistency in sleeping times can influence body fat.
Researchers found that:
The difference in body weight was greater with more variation in sleep pattern. Women whose sleep patterns varied by 90 minutes a night had higher body fat than those whose sleep varied by 60 minutes or less on average. Body fat also varied with sleep quantity; women who slept between 8 and 8.5 hours a night had the lowest body fat. The greatest effect was seen in women who woke up at the same time every morning seven days a week.
Although this was a small, short duration study with study participants selected from a limited pool (only young, only college educated, etc.) and was not blinded or controlled, other studies have shown that sleep has an effect on physical activity, appetite, and the hormones that control appetite and metabolism. According to those studies skimping on sleep boosts production of ghrelin, (a hormone that controls food cravings) and decreases production of leptin, (a hormone that helps prevent over-eating). A body of research conducted over the last few years that ties quality and quantity of sleep to weight loss and better weight control included a randomized trial published in the journal Obesity which found that among overweight and obese women ages 35 to 55 engaged in a weight loss programs, getting an adequate amount of good quality sleep increased the chance of weight loss success by 33 percent.
While researchers don’t know exactly how sleep schedules affect body mass and fat, consistent sleep patterns are part of good sleep hygiene. Click here to learn more about improving your sleep and the importance of sleep hygiene.
The report was published online in the November issue of the American Journal of Health Promotion.
References:
Forbes;Change Your Sleep Schedule To Lose Weight, Study Shows; Melanie Haiken,11/21/2013
Steady Sleep Schedule May Help Keep Weight Off; Philly.com; Steven Reinberg, 11/21/2013
Researchers found that:
- Less than 6.5 hours of sleep or more than 8.5 hours of sleep was linked to higher body fat
- High quality sleep was associated with lower body fat, while poor sleep correlated with higher body fat
- Consistent wake times and going to sleep at the same time every day (particularly the consistent wake time) were most strongly linked with lower body fat
The difference in body weight was greater with more variation in sleep pattern. Women whose sleep patterns varied by 90 minutes a night had higher body fat than those whose sleep varied by 60 minutes or less on average. Body fat also varied with sleep quantity; women who slept between 8 and 8.5 hours a night had the lowest body fat. The greatest effect was seen in women who woke up at the same time every morning seven days a week.
Although this was a small, short duration study with study participants selected from a limited pool (only young, only college educated, etc.) and was not blinded or controlled, other studies have shown that sleep has an effect on physical activity, appetite, and the hormones that control appetite and metabolism. According to those studies skimping on sleep boosts production of ghrelin, (a hormone that controls food cravings) and decreases production of leptin, (a hormone that helps prevent over-eating). A body of research conducted over the last few years that ties quality and quantity of sleep to weight loss and better weight control included a randomized trial published in the journal Obesity which found that among overweight and obese women ages 35 to 55 engaged in a weight loss programs, getting an adequate amount of good quality sleep increased the chance of weight loss success by 33 percent.
While researchers don’t know exactly how sleep schedules affect body mass and fat, consistent sleep patterns are part of good sleep hygiene. Click here to learn more about improving your sleep and the importance of sleep hygiene.
The report was published online in the November issue of the American Journal of Health Promotion.
References:
Forbes;Change Your Sleep Schedule To Lose Weight, Study Shows; Melanie Haiken,11/21/2013
Steady Sleep Schedule May Help Keep Weight Off; Philly.com; Steven Reinberg, 11/21/2013
Friday, November 8, 2013
Don't let Snoring Break Your Heart!
For years people have thought of snoring as nothing more than a simple annoyance during the night: snoring is so common that we do not view it as a medical problem. Recent statistics suggest that this seemingly simple noise problem may in fact increase the risk of high blood pressure, stroke, heart attack, and daytime sleepiness.
Snoring typically occurs when the tongue and throat muscles relax during sleep causing the airway space in the back of the throat to narrow. Breathing through a narrow airway causes a vacuum that pulls on the throat's soft tissue causing it to vibrate, which creates the snoring sound. This vacuum in the throat also spreads to the chest where the heart is located, causing a strain on the heart and the possibility for oxygen in the bloodstream to drop to dangerously low levels. When these factors occur night after night, year after year, they instigate the problems listed above. Additionally, new studies have also shown OSA causes increased insulin resistance resulting in poorly controlled diabetes.
Studies have demonstrated that in many people, snoring can cause an increase in chest pressures which can influence blood flow in the heart and lungs. This may be the cause of some of the medical problems in people who snore.
CSMA's sleep centers throughout Greater Houston provide treatment to patients sufferering from snoring and obstructive sleep apnea disorders. For more information on how to stop snoring and obtain help for sleep apnea call us today at (281) 407-6222.
Many people who snore have another problem known as sleep apnea. Apnea is a Greek word, which means, "want to breathe." People with obstructive sleep apnea have pauses in their breathing while asleep. These pauses in breathing occur when the airway collapses during sleep. After a few seconds the person briefly awakens, frequently producing a grunting, gasping, or snorting sound.
Obstructive sleep apnea is more common in obese people and more common in men, but it is not just obesity that can cause this problem. People with a small jaw, large tongue, or large tonsils are at higher risk of having this problem as well. In fact, any condition which can narrow the opening in the back of the throat or possibly the nasal passages can increase the risk of obstructive sleep apnea.
It is important to know the consequences of this problem if left untreated. Some of the more common problems associated with obstructive sleep apnea are excessive daytime sleepiness and an increased risk of high blood pressure, heart attacks and stroke.
What can someone do if they want to know if they have Sleep Apnea?
See your physician and ask about being referred to a sleep disorders center. This is a special testing facility that evaluates people for sleeping problems. If your doctor does not feel this is necessary, don't be discouraged. Most physicians have not been taught very much about sleep medicine in medical school and therefore may not recognize this problem in their patients. Be persistent. You can be seen by a sleep specialist and, if needed, a sleep study can be performed on you during the night.What can be done if a person snores or has Sleep Apnea?
The most effective treatment to date for sleep apnea is called nasal CPAP (Continuous Positive Airway Pressure). An individual wears a mask on their nose at night that administers air pressure, keeping the upper airway open. This allows the individual to breathe throughout the night without repetitive awakenings. If a person only snores and does not suffer from excessive daytime sleepiness, then CPAP is not the appropriate treatment.Dental appliances have been used for snoring. Sometimes these devices can also prevent apnea as well. Studies have demonstrated that dental appliances work for snoring and sleep apnea, but not in all patients. Surgery has been used to treat these problems. The most frequently performed surgery is a procedure where the soft tissue in the back of the throat including the uvula is cut away or reduced in size with a new microwave needle or a laser. Although this may work well for snoring, unfortunately most patients who have sleep apnea are not adequately treated with these procedures. There are other more extensive surgeries that can be performed for sleep apnea.
A sleep specialist who is very familiar with these
procedures should explain them to you. If you snore at night and think
you might have sleep apnea, contact your doctor. If your doctor is not
familiar with this type of problem, have him or her contact us directly.
For more information on Snoring, Sleep Apnea and treatment options in the greater Houston area, visit www.HoustonSleep.net
Saturday, October 26, 2013
Comprehensive Sleep Medicine Associates, PA welcomes Dr. Gerard Joseph Meskill as Staff Neurologist and Sleep Disorders Specialist.
Dr. Meskill is a neurologist and sleep disorders specialist. He
completed his neurology residency at the Hofstra-North Shore Long Island
Jewish School of Medicine. The North Shore Long Island Jewish
healthcare system is the largest provider of patient care in New York
City, with 16 hospitals serving a population of 7 million people
spanning three boroughs of New York City and Long Island. The two
flagship hospitals of that system, North Shore University Hospital and
Long Island Jewish Medical Center, serve as the tertiary care centers
for the entire system. Training almost exclusively in those two
hospitals, Dr. Meskill was exposed to the full breadth of neurologic
disorders, ranging from critical care to outpatient cases, as well as
some of the rarest disease processes to common ailments.
After residency, Dr. Meskill switched coasts to continue his training at Stanford University School of Medicine's Sleep Disorders fellowship program. Founded by Dr. William Dement, Stanford's program is recognized internationally as the birthplace of the field and is considered the world's best academic sleep program. Dr. Meskill trained under many of the most recognized innovators in sleep medicine, such as Dr. Dement, considered the father of sleep medicine; Dr. Emmanuel Mignot, the chairman of the program and the world authority on Narcolepsy; and Dr. Christian Guilleminault, one of the world's most published authors in the field of sleep and a major contributor to the discovery of the physiologic mechanisms behind Obstructive Sleep Apnea. Due to Stanford's international reputation and extensive clinical case diversity, Dr. Meskill routinely evaluated and treated both common and rare sleep disorders, ranging from Obstructive Sleep Apnea to Kleine-Levin Syndrome.
Dr. Meskill treats a wide range of neurologic disorders, but like his colleague and fellow Stanford graduate, Dr. Jerald Simmons, he spends majority of his time evaluating and treating sleep disorders. This includes the full spectrum of sleep-disordered breathing, from Upper Airway Resistance Syndrome to Obstructive Sleep Apnea, as well as nocturnal bruxism (teeth clenching/grinding), pediatric and adult ADD/ADHD, Fibromyalgia, Chronic Fatigue Syndrome, TMJ/TMD, Narcolepsy, Restless Legs Syndrome, Periodic Limb Movement Disorder, Epilepsy, and many other disorders. Many of these disorders are related to or are exacerbated by obstructive respirations during sleep. Like Dr. Simmons, Dr. Meskill is trained in the implementation and interpretation of esophageal manometry, which is considered the gold standard measure for detecting sleep-disordered breathing events.
Dr. Meskill is dedicated to improving the standard of care for sleep and neurologic disorders in the Houston area, as well as promoting better understanding of these fields through community education and collaboration with primary care physicians, subspecialists, and community dentists.
Dr. Meskill has recently published two articles in Huffington Post "Healthy Living": Episodic Excessive Sleepiness in Teens May Represent Kleine-Levin (April 09 2013) and Nocturnal Teeth Grinding May Suggest a Sleep Disorder (October 24 2013).
After residency, Dr. Meskill switched coasts to continue his training at Stanford University School of Medicine's Sleep Disorders fellowship program. Founded by Dr. William Dement, Stanford's program is recognized internationally as the birthplace of the field and is considered the world's best academic sleep program. Dr. Meskill trained under many of the most recognized innovators in sleep medicine, such as Dr. Dement, considered the father of sleep medicine; Dr. Emmanuel Mignot, the chairman of the program and the world authority on Narcolepsy; and Dr. Christian Guilleminault, one of the world's most published authors in the field of sleep and a major contributor to the discovery of the physiologic mechanisms behind Obstructive Sleep Apnea. Due to Stanford's international reputation and extensive clinical case diversity, Dr. Meskill routinely evaluated and treated both common and rare sleep disorders, ranging from Obstructive Sleep Apnea to Kleine-Levin Syndrome.
Dr. Meskill treats a wide range of neurologic disorders, but like his colleague and fellow Stanford graduate, Dr. Jerald Simmons, he spends majority of his time evaluating and treating sleep disorders. This includes the full spectrum of sleep-disordered breathing, from Upper Airway Resistance Syndrome to Obstructive Sleep Apnea, as well as nocturnal bruxism (teeth clenching/grinding), pediatric and adult ADD/ADHD, Fibromyalgia, Chronic Fatigue Syndrome, TMJ/TMD, Narcolepsy, Restless Legs Syndrome, Periodic Limb Movement Disorder, Epilepsy, and many other disorders. Many of these disorders are related to or are exacerbated by obstructive respirations during sleep. Like Dr. Simmons, Dr. Meskill is trained in the implementation and interpretation of esophageal manometry, which is considered the gold standard measure for detecting sleep-disordered breathing events.
Dr. Meskill is dedicated to improving the standard of care for sleep and neurologic disorders in the Houston area, as well as promoting better understanding of these fields through community education and collaboration with primary care physicians, subspecialists, and community dentists.
Dr. Meskill has recently published two articles in Huffington Post "Healthy Living": Episodic Excessive Sleepiness in Teens May Represent Kleine-Levin (April 09 2013) and Nocturnal Teeth Grinding May Suggest a Sleep Disorder (October 24 2013).
New Study Shows That Sleep "Cleans the Brain".
A new study funded by the National Institute of Neurological Disorders and Stroke (NINDS) and published in Science shows that sleep increases the flow of cerebrospinal fluid in the brain which in turn flushes harmful waste proteins known as metabolites from the brain. Maiken Nedergaard, M.D., D.M.Sc. professor of neurosurgery at the University of Rochester and an author of the study discovered the cleaning process while studying the brains of sleeping mice: dubbed the glymphatic system, it pumps cerebral spinal fluid (CSF) through the spaces around the brain
cells, flushing waste into the circulatory system where it eventually
makes its way to the liver.
Researchers studied the system by injecting dye into the CSF of mice and then observing it as it flowed through the brain using two-photon microscopy- a new imaging technology that allows scientists to see deep inside living tissue- while simultaneously monitoring electrical brain activity. The dye flowed rapidly when the mice were either asleep or anesthetized but barely flowed at all when the same mice were awake.
The researchers also discovered that during sleep brain cells contract, increasing the space between the cells by as much as 60 percent and allowing the spinal fluid to wash more freely through the brain tissue.
One of the waste products of the brain is the protein amyloid-beta, which accumulates and forms plaques in the brains of Alzheimer’s patients. Researchers at Washington University in St. Louis had previously shown that levels of amyloid-beta in mice brains dropped during sleep because of a decrease in production of the protein.“That was an observation that inspired our work,” says Nedergaard. Research in humans has shown that levels of amyloid-beta decline during sleep, as it does in mice, but it’s not yet known if the mechanisms are the same as in mice.
References:
Maiken Nedergaard, M.D., D.M.Sc.
U.S. Department of Health and Human Services: The National Institutes of Health (NIH)
NPR: brains-sweep-themselves-clean-of-toxins-during-sleep
NBC News: good-nights-sleep-scrubs-your-brain-clean
Researchers studied the system by injecting dye into the CSF of mice and then observing it as it flowed through the brain using two-photon microscopy- a new imaging technology that allows scientists to see deep inside living tissue- while simultaneously monitoring electrical brain activity. The dye flowed rapidly when the mice were either asleep or anesthetized but barely flowed at all when the same mice were awake.
The researchers also discovered that during sleep brain cells contract, increasing the space between the cells by as much as 60 percent and allowing the spinal fluid to wash more freely through the brain tissue.
One of the waste products of the brain is the protein amyloid-beta, which accumulates and forms plaques in the brains of Alzheimer’s patients. Researchers at Washington University in St. Louis had previously shown that levels of amyloid-beta in mice brains dropped during sleep because of a decrease in production of the protein.“That was an observation that inspired our work,” says Nedergaard. Research in humans has shown that levels of amyloid-beta decline during sleep, as it does in mice, but it’s not yet known if the mechanisms are the same as in mice.
References:
Maiken Nedergaard, M.D., D.M.Sc.
U.S. Department of Health and Human Services: The National Institutes of Health (NIH)
NPR: brains-sweep-themselves-clean-of-toxins-during-sleep
NBC News: good-nights-sleep-scrubs-your-brain-clean
Monday, October 14, 2013
New study suggests that children without regular bedtimes have more behavioral problems.
Researchers from University College London recently completed a long-term study of babies born in the UK in 2000 to 2002, which regularly surveyed parents about sleep and behavioral problems. After analyzing data for over 10,000 children they discovered that children without a regular bedtime tended to
score worse on a measure of behavior problems such as acting unhappy,
getting into fights and being inconsiderate.
In three year olds, close to 20 percent of parents said their child sometimes or never went to bed at a consistent time. That fell to 9 percent among five year olds and 8 percent for seven year olds: at seven those without a regular bedtime scored an 8.5, on average, based on their mothers' reports. That compared to scores between 6.3 and 6.9 for kids who had a consistent bedtime before 9 p.m.
The assessment is scored from 0 to 40, with higher scores indicating more problems. Researchers said one to two points represents a small or moderate difference, but is "meaningful."
Children with attention-deficit/hyperactivity disorder or an autism spectrum disorder were not included in the study. Teachers of seven year olds were also asked to report on their, and gave worse scores to children who didn't have a regular bedtime. Although the researchers accounted for other parent characteristics and family habits, it's still possible kids' behavior problems weren't directly caused by irregular bedtimes.
Nonetheless, the effects that a regular sleep schedule have on your "biological clock" have been well documented. Yvonne Kelly, who led the study says that "If you are constantly changing the amounts of sleep you get or the different times you go to bed, it's likely to mess up your body clock. That has all sorts of impacts on how your body is able to work the following day."
Kids whose parents said they had non-regular bedtimes on every survey growing up had the most behavioral issues, but when children went from having a non-regular bedtime to a regular bedtime on the following survey their behavior scores improved.
References:
Pediatrics (online October 14, 2013)
Non-regular bedtimes tied to kids' behavior problems (Reuters)
In three year olds, close to 20 percent of parents said their child sometimes or never went to bed at a consistent time. That fell to 9 percent among five year olds and 8 percent for seven year olds: at seven those without a regular bedtime scored an 8.5, on average, based on their mothers' reports. That compared to scores between 6.3 and 6.9 for kids who had a consistent bedtime before 9 p.m.
The assessment is scored from 0 to 40, with higher scores indicating more problems. Researchers said one to two points represents a small or moderate difference, but is "meaningful."
Children with attention-deficit/hyperactivity disorder or an autism spectrum disorder were not included in the study. Teachers of seven year olds were also asked to report on their, and gave worse scores to children who didn't have a regular bedtime. Although the researchers accounted for other parent characteristics and family habits, it's still possible kids' behavior problems weren't directly caused by irregular bedtimes.
Nonetheless, the effects that a regular sleep schedule have on your "biological clock" have been well documented. Yvonne Kelly, who led the study says that "If you are constantly changing the amounts of sleep you get or the different times you go to bed, it's likely to mess up your body clock. That has all sorts of impacts on how your body is able to work the following day."
Kids whose parents said they had non-regular bedtimes on every survey growing up had the most behavioral issues, but when children went from having a non-regular bedtime to a regular bedtime on the following survey their behavior scores improved.
References:
Pediatrics (online October 14, 2013)
Non-regular bedtimes tied to kids' behavior problems (Reuters)
Saturday, October 5, 2013
Treating Snoring Problems
SNORING Threatens Your Health!
Snoring can be a sign of Obstructive Sleep Apnea (OSA), which has been linked to high blood pressure, heart disease and an increased risk of heart attacks and stroke.For years people have thought of snoring as nothing more than a simple annoyance during the night: snoring is so common that we do not view it as a medical problem.
Snoring typically occurs when the tongue and throat muscles relax during sleep causing the airway space in the back of the throat to narrow. Breathing through a narrow airway causes a vacuum that pulls on the throat's soft tissue causing it to vibrate, which creates the snoring sound.
This vacuum in the throat also spreads to the chest where the heart is located, causing a strain on the heart and the possibility for oxygen in the bloodstream to drop to dangerously low levels.
When these factors occur night after night, year after year, they instigate the problems listed above. Additionally, new studies have also shown OSA causes increased insulin resistance resulting in poorly controlled diabetes.
Studies have demonstrated that in many people, snoring can cause an increase in chest pressures which can influence blood flow in the heart and lungs. This may be the cause of some of the medical problems in people who snore.
Many people who snore have another problem known as sleep apnea. Apnea is a Greek word, which means, "want to breathe." People with obstructive sleep apnea have pauses in their breathing while asleep. These pauses in breathing occur when the airway collapses during sleep. After a few seconds the person briefly awakens, frequently producing a grunting, gasping, or snorting sound.
Obstructive sleep apnea is more common in obese people and more common in men, but it is not just obesity that can cause this problem. People with a small jaw, large tongue, or large tonsils are at higher risk of having this problem as well. In fact, any condition which can narrow the opening in the back of the throat or possibly the nasal passages can increase the risk of obstructive sleep apnea.
It is important to know the consequences of this problem if left untreated.
Some of the more common problems associated with obstructive sleep apnea are excessive daytime sleepiness and an increased risk of high blood pressure, heart attacks and stroke.
What can someone do if they want to know if they have Sleep Apnea?
See your physician and ask about being referred to a sleep disorders center. This is a special testing facility that evaluates people for sleeping problems. If your doctor does not feel this is necessary, don't be discouraged. Most physicians have not been taught very much about sleep medicine in medical school and therefore may not recognize this problem in their patients. Be persistent. You can be seen by a sleep specialist and, if needed, a sleep study can be performed on you during the night.
What can be done if a person snores or has Sleep Apnea?
The most effective treatment to date for sleep apnea is called nasal CPAP (Continuous Positive Airway Pressure). An individual wears a mask on their nose at night that administers air pressure, keeping the upper airway open. This allows the individual to breathe throughout the night without repetitive awakenings. If a person only snores and does not suffer from excessive daytime sleepiness, then CPAP is not the appropriate treatment.Dental appliances have been used for snoring. Sometimes these devices can also prevent apnea as well. Studies have demonstrated that dental appliances work for snoring and sleep apnea, but not in all patients. Surgery has been used to treat these problems. The most frequently performed surgery is a procedure where the soft tissue in the back of the throat including the uvula is cut away or reduced in size with a new microwave needle or a laser. Although this may work well for snoring, unfortunately most patients who have sleep apnea are not adequately treated with these procedures. There are other more extensive surgeries that can be performed for sleep apnea.
Comprehensive Sleep Medicine Associates, PA. (CSMA) treats the full spectrum of sleep disturbances in patients ranging from pediatrics to geriatrics.
A sleep specialist who is very familiar with these procedures should explain them to you. If you snore at night and think you might have sleep apnea, contact your doctor. If your doctor is not familiar with this type of problem, have him or her contact us directly.If you or someone you know has one or more of these symptoms, a sleep disorder may be the cause and an evaluation is needed; help is available by Dr. Jerald H. Simmons and his dedicated team at CSMA. Dr. Simmons established CSMA as an outreach program in the Greater Houston area and now has facilities in the Houston Medical Center, Sugar Land and The Woodlands. The Sleep Medicine Specialists at CSMA can help you determine the cause of your sleep problems and restore night after night of healthy, restful sleep.
Sunday, September 29, 2013
Research suggests that some fears may be overcome through a combination of scent and sleep.
Scientists at Northwestern University say they have lowered levels of
fear in people by using certain odors to trigger and rechannel
frightening memories into harmless ones during deep sleep.
Researchers created an artificial "fear" in 15 healthy subjects by showing them photos of different faces and applying electric shocks when two of the photos were shown. Conditioning also included associating each face with a particular odor.
Fear was detected through a process similar to a lie detector test, which measured small amounts of sweat in the skin. After several trials the participants became afraid of the face and the smell associated with it; the scent was then used to trigger "fear memories" during deep sleep in order to allow patients to avoid the stress of conscious terror.
The subjects then napped for a couple of hours. Whenever they fell into a deep phase known as slow-wave sleep, they were given the odor associated with one of the two "scary" faces, but without the accompanying jolts.
The subjects were allowed to stay in slow-wave sleep for periods ranging from five to 40 minutes: the effect was strongest for those who slept for longest.
After the subjects awoke, they again went through the process of being shown the series of different faces. This time they weren’t as afraid of the face with the scent they had been exposed to during sleep, however they remained fearful of the other, whose associated odor they hadn’t been exposed to during sleep.
Also, those who were exposed to the scent for the longest total time while sleeping were less afraid of the face than those who had smelled it for a short time.
The subjects did not know what happened during their sleep.
Researchers also used fMRI (functional magnetic resonance imaging). The fMRI results showed changes in regions associated with memory, such as the hippocampus, and changes in patterns of brain activity in regions associated with emotion, such as the amygdala. These brain changes reflected a decrease in reactivity that was specific to the targeted face image associated with the scent presented during sleep.
Sleep plays a key role in memory consolidation, which involves parts of the brain replaying the events of the day and choosing which parts to store for safekeeping and which to forgo.
Dr. Jay Gottfried, PhD., senior author of the study, says "Sleep sort of stamps memories in more strongly: that’s when a lot of memory formation can take place.”
People with phobias are already commonly treated with "gradual exposure" therapy while they are awake, where they are exposed to the thing they are frightened of in incremental degrees. This study suggests that the theory could be extended to therapy while they are in slow-wave, or deep, sleep.
"It's a novel finding," said Katherina Hauner, a postdoctoral fellow in neurology at Northwestern University Feinberg School of Medicine. "We showed a small but significant decrease in fear. If it can be extended to pre-existing fear, the bigger picture is that, perhaps, the treatment of phobias can be enhanced during sleep."
The study was published in the Sept. 22 journal Nature Neuroscience.
References:
washingtonpost.com
sciencedaily.com
bbc.co.uk
Researchers created an artificial "fear" in 15 healthy subjects by showing them photos of different faces and applying electric shocks when two of the photos were shown. Conditioning also included associating each face with a particular odor.
Fear was detected through a process similar to a lie detector test, which measured small amounts of sweat in the skin. After several trials the participants became afraid of the face and the smell associated with it; the scent was then used to trigger "fear memories" during deep sleep in order to allow patients to avoid the stress of conscious terror.
The subjects then napped for a couple of hours. Whenever they fell into a deep phase known as slow-wave sleep, they were given the odor associated with one of the two "scary" faces, but without the accompanying jolts.
The subjects were allowed to stay in slow-wave sleep for periods ranging from five to 40 minutes: the effect was strongest for those who slept for longest.
After the subjects awoke, they again went through the process of being shown the series of different faces. This time they weren’t as afraid of the face with the scent they had been exposed to during sleep, however they remained fearful of the other, whose associated odor they hadn’t been exposed to during sleep.
Also, those who were exposed to the scent for the longest total time while sleeping were less afraid of the face than those who had smelled it for a short time.
The subjects did not know what happened during their sleep.
Researchers also used fMRI (functional magnetic resonance imaging). The fMRI results showed changes in regions associated with memory, such as the hippocampus, and changes in patterns of brain activity in regions associated with emotion, such as the amygdala. These brain changes reflected a decrease in reactivity that was specific to the targeted face image associated with the scent presented during sleep.
Sleep plays a key role in memory consolidation, which involves parts of the brain replaying the events of the day and choosing which parts to store for safekeeping and which to forgo.
Dr. Jay Gottfried, PhD., senior author of the study, says "Sleep sort of stamps memories in more strongly: that’s when a lot of memory formation can take place.”
People with phobias are already commonly treated with "gradual exposure" therapy while they are awake, where they are exposed to the thing they are frightened of in incremental degrees. This study suggests that the theory could be extended to therapy while they are in slow-wave, or deep, sleep.
"It's a novel finding," said Katherina Hauner, a postdoctoral fellow in neurology at Northwestern University Feinberg School of Medicine. "We showed a small but significant decrease in fear. If it can be extended to pre-existing fear, the bigger picture is that, perhaps, the treatment of phobias can be enhanced during sleep."
The study was published in the Sept. 22 journal Nature Neuroscience.
References:
washingtonpost.com
sciencedaily.com
bbc.co.uk
Monday, September 23, 2013
January 24 & 25 Houston Sleep Medicine Conferences
The Sleep Education Consortium is pleased to present the
10th Annual Sleep Education Consortium Conference:
Problem Based Sleep Medicine Course to Enhance Your Clinical Practice: Establishing a Differential Diagnosis and Treatment Plan for Sleep Disorders
January 25, 2014 at the Houston Medical Center Marriott
This conference is designed to present important clinical
information on sleep disorders that can be implemented into the practice
of primary care physicians. Materials will be presented in a case based
fashion with specific clinical cases that exemplify the type of
problems presented to most practitioners.
Course materials will include reference materials and assessment
tools such as questionnaires that can be used in primary care settings.
There will be discussions on how to respond to the results provided from
a diagnostic sleep study, as well as the indications for obtaining such
tests.
This activity has been planned and implemented in accordance with the Essential Areas and Policies of the Accreditation Council for continuing Medical Education through the joint sponsorship of the Texas Medical Association and The Sleep Education Consortium, Inc. The Texas Medical Association (TMA) is accredited by the Accreditation Council for continuing Medical Education (ACCME) to provide continuing medical education for physicians. The TMA designates this live activity for a maximum of 8 AMA PRA Category 1 Credits™. Physicians should only clam credit commensurate with the extent of their participation in the activity.
Register Now at www.houstonsleep.org
The Growing Role of the Dentist in Sleep Disorders Medicine: Integrating the Dentist into the Medical Treatment Team
January 24 and 25, 2014 at the Houston Medical Center Marriott
This conference architects the growing link between dentistry and
sleep medicine, and it will become clear how the dentist can play a
larger role in the overall health of patients.
Gain the knowledge you need to address your patient’s sleep concerns in a
two day comprehensive course tailored to provide dental professionals
with the essentials to build their dental practice in this evolving area
of dentistry.
The Houston Sleep Education Consortium presents a unique opportunity
to learn about the dentists’ role in sleep disorders treatment (we
don't just treat "a" disorder).
In an effort to provide the best educational experience the
conference dedicates one day of lectures specifically designed to
address the educational needs of the D.D.S., and the second day of
lectures has a Break Out Session for the dental support staff. Also, the
second day is open to all health care professionals and has a broader
range of sleep related lecture topics.
Registration is available for the first day alone or both days
(highly recommended).
By addressing the patients' questions regarding sleep issues, the
dentist and support staff can be grounded in the broader aspect of sleep
disorders on a basic level. Attending both days of the conference will
allow the dentist and support staff to become familiar with a multitude
of sleep problems, and they can be more responsive to questions patients
may ask as the dentist screens for sleep disorders within their
practice.
The educational methods will include lectures, Q&A and panel
discussion.
Obtain 8 hours of continuing education credit for each day of
attendance of this exciting and informative seminar that is sure to
expand your practice.
A CE Course for a total 16 hours of AGD and ADA-CERP approved credits.
Register Now at www.dentalsleepconference.com
For more information please contact:
The Sleep Education Consortium Inc.,
PO Box 16820, Sugar Land, TX 77496.
PO Box 16820, Sugar Land, TX 77496.
For Hotel Reservations:
Houston Marriott at the Texas Medical Center
6580 Fannin Street
Houston, Texas 77030
Phone: 1-(713)-796-0080
Fax: 1-(713)-770-8100
Houston Marriott at the Texas Medical Center
6580 Fannin Street
Houston, Texas 77030
Phone: 1-(713)-796-0080
Fax: 1-(713)-770-8100
Monday, February 11, 2013
Possible Texas Dental Law Changes May Enhance Collaboration of Physicians & Dentists in Treating Obstructive Sleep Apnea (OSA)
The Texas State Board of Dental Examiners does not recognize OSA diagnosis and treatment within the current scope of dentistry and Houston sleep expert Jerald H. Simmons, MD recognizes the partnerships needed to treat this sleep disorder. This team-based care will be the focus at the 9th Annual Sleep Education Consortium's (SEC) conference, Feb 8-9, 2013 in Houston that brings the dentist and the physician together for continuing education classes, said SEC's Founding-Director, Dr. Simmons.
Obstructive sleep apnea (OSA) is a medical condition where repeated narrowing of the throat occurs during sleep which either partially or completely blocks the airway. This blockage can repeatedly stop breathing for many that lasts 20 seconds or longer. OSA can occur at any age and it is estimated that more than 12 million Americans have this disorder. According to the American Academy of Sleep Medicine about 80 to 90 percent of adults with OSA remain undiagnosed.Many physicians are not recognizing the problem leaving so many untreated. This has created a niche for those dentists who may recognize the symptoms of OSA and step-in to fill this void. However, many dentists are now providing services to patients for OSA, a medical condition, which is technically outside of the scope of dentistry. Recognizing this trend, the Texas State Board of Dental Examiners (TSBDE) is evaluating the situation to determine a formal position on this topic. Jerald H. Simmons, MD, who is triple board-certified by the American Board of Sleep Medicine, American Board of Psychiatry and Neurology and the American Board of Clinical Neurophysiology presented to the dental board his expert opinion at their January 25th Austin meeting.
To view the full article please visit our PRWEB release.
For more information on Obstructive Sleep Apnea visit www.dr-jhsimmons.com
Subscribe to:
Posts (Atom)