Information on the treatment of Snoring, Sleep Apnea, Excessive Daytime Sleepiness and other Sleep Disorders by Houston, Texas Neurologist and Sleep Medicine Specialist Jerald Simmons M.D. If you suffer from sleep problems, Dr. Simmons and his staff at CSMA can provide relief with three state of the art sleep medicine centers in the greater Houston area.

Monday, December 23, 2013
New Gallup Poll Data Suggests 40% of Americans Don't Get Enough Sleep
A new Gallup poll shows that 40% of Americans get less than seven hours of sleep per night- a figure largely unchanged from the 1990s and 2000s.
The poll is based on telephone interviews conducted Dec. 5-8, 2013, with a random sample of 1,031 adults, aged 18 and older, living in all 50 U.S. states and the District of Columbia.
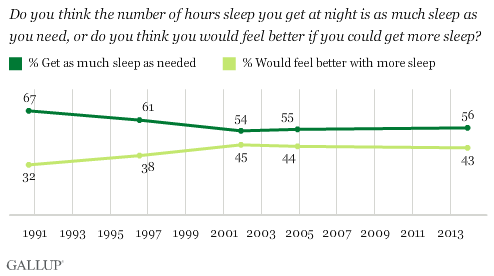
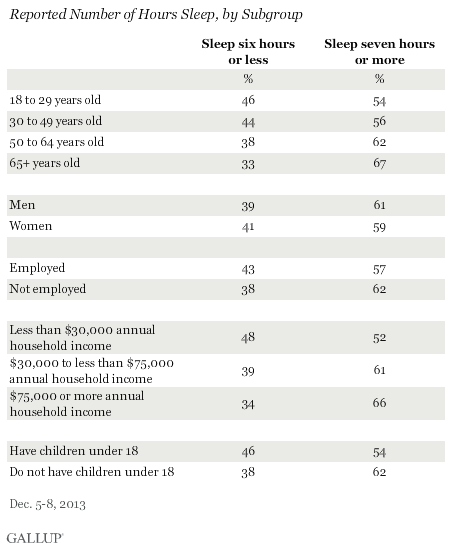
56% of Americans say they get as much sleep as needed, while 43% say they would feel better if they got more sleep. The percentage who say they get sufficient sleep has been in the mid-50% range since 2001, but was much higher in 1990. Americans aged 65 and older report getting the most sleep, with 67% getting seven or more hours per night. Each younger age group gets less sleep, down to 54% of 18- to 29-year-olds who report getting seven or more hours. Nearly half of 18- to 29-year-olds get less than the recommended amount of sleep.
Medical studies have related a lack of sleep to health problems and cognitive impairment: experts typically recommend seven to nine hours sleep for adults.
The indirect cost of sleep disorders is estimated at 41 billion dollars per year from lost productivity, 17 to 27 billion dollars per year from motor vehicle accidents, 7 billion dollars per year in work-related accidents and 2 to 4 billion dollars per year in home and public accidents (Stoller MK Clin Ther 1994:16 873-897). These figures do not even take into account the added morbidity caused by the physiologic impact from sleep disorders. Unfortunately, Sleep, a process which consumes about one third of our life and which has a spectrum of abnormalities which can hinder our daily living, has received so little attention in our medical education system.
For more information on the importance of proper sleep hygiene, The Societal Sleep Problem and sleep related illness please visit the HoustonSleep.Net.
References:
Gallup.com: In U.S., 40% Get Less Than Recommended Amount of Sleep
Methodology, full question results and trend data
Friday, December 13, 2013
Poor Sleep is Frequently at the Root of Fibromyalgia
For decades, doctors have been challenged in treating patients with a condition known as fibromyalgia. Patients with fibromyalgia complain of pain in various parts of their body, and evaluation by the doctor does not identify any physical cause. There are no inflammation or arthritic changes in the bones to explain the daily difficulties with pain. More than 12 million Americans have been labeled with this diagnosis and treatment options have been limited; for the most part it has consisted of pain medications or medications that dull the nerve pain transmission from around the body to the brain. These medications frequently cause side effects including drowsiness, and their benefits lessen over time.
A new direction in the management of fibromyalgia stems from our growing knowledge of this mysterious disorder. Dr. Jerald H. Simmons, neurologist and founding director of Comprehensive Sleep Medicine Associates (CSMA), says that fibromyalgia is a condition in which the brain's pain-filtering system is fatigued and does not function correctly: "Our brains constantly filter out signals coming in from the nerve fibers throughout the body. This allows us to function without feeling every little impulse coming from all of the nerves. When we sleep, this filter in our brain restores itself in preparation to function throughout the next day. When we are sleep-deprived or have not gotten proper sleep, the filter system begins to malfunction and signals from the nerves that should have been filtered out instead get into the brain and create the sensation of pain."
Another way to describe this is that our pain threshold is lowered by poor sleep, and this relationship between sleep and pain has become increasingly dear. As it turns out, many patients with sleep disorders who have also been identified as suffering from fibromyalgia experience resolution of their fibromyalgia pain as a result of treatment of their sleep disorder. The link between sleep and other conditions has become increasingly clear. "If we improve sleep in fibromyalgia patients, we have seen that the pain improves as well," Dr. Simmons says. "Common sleep disturbances such as obstructive sleep apnea, restless legs syndrome or upper airway resistance syndrome seem to be underlying causes of patients' fragmented sleep. Many of these patients also complain of chronic fatigue syndrome, further implicating sleep disruption as a contributing factor. I have had excellent results from identifying the root of the disrupted sleep and then treating the sleep disturbance."
Dr. Simmons uses a new approach to treat patients with fibromyalgia that have not been identified as having another sleep disorder; it involves Zyrem, a medication originally used for treating narcolepsy. "Now that I'm on Zyrem, I feel better than I have in 20 years," said Nancy Schweining, one of Dr. Simmons' patients. "My pain is gone and I feel like I have my life back." Dr. Simmons expects more doctors to recognize the proper use of this medication, which he said enhances Sleep Wave sleep in patients with fibromyalgia.
If you or someone you know suffers from fibromyalgia, consider the possibility that poor sleep may be at the root of the condition. Evaluation can be provided by Dr. Simmons and his staff at CSMA's sleep centers throughout Greater Houston by calling 281-407-6222 or by visiting www.HoustonSleep.Net.
Subscribe to:
Posts (Atom)